Gastric Bypass Surgery: A Patient-Friendly Guide
Overview of the Procedure
What is Gastric Sleeve Surgery?
Gastric sleeve surgery, also known as sleeve gastrectomy, is a surgical weight-loss procedure that involves removing about 75-80% of the stomach, leaving a smaller, sleeve-shaped stomach.
It helps in weight loss by reducing stomach size, making patients feel full with less food, and altering hunger-related hormones.


Why is it Performed?
To treat severe obesity and its related health issues such as diabetes, high blood pressure, and sleep apnea.
Recommended for individuals with a BMI of 40 or higher (or 35+ with obesity-related conditions).
Is it Surgical, Non-Surgical, or Minimally Invasive?
It is a surgical procedure performed laparoscopically (small incisions, minimally invasive).
Alternative Treatments
Diet & exercise programs (for mild obesity)
Medication-assisted weight loss
Gastric bypass surgery (another bariatric procedure that reroutes digestion)
Endoscopic sleeve gastroplasty (a non-surgical alternative that reduces stomach size using sutures)
Benefits of the Procedure
Health Conditions It Addresses
Significant weight loss, helping with obesity-related diseases
Lower blood sugar levels, improving or resolving Type 2 diabetes
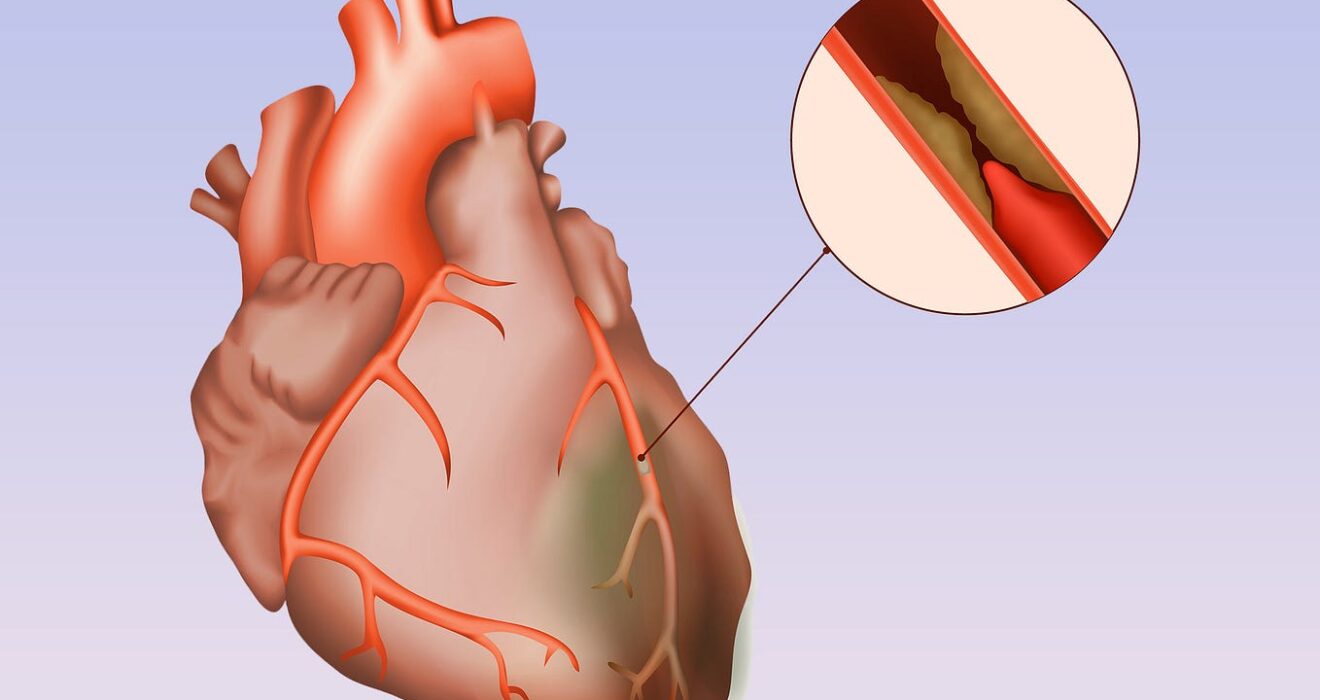
Reduced risk of heart disease, stroke, and high blood pressure
Improved sleep apnea symptoms
Better mobility and reduced joint pain
Expected Improvements in Quality of Life
Increased energy and mobility
Improved mental health, self-esteem, and confidence
Enhanced overall well-being and longevity
Success Rates & Effectiveness
Patients typically lose 50-70% of excess body weight within the first 12-18 months
High long-term success rates with proper diet and lifestyle changes
Preparation Before the Procedure
Pre‑Procedure Requirements
Medical evaluation (blood tests, imaging, nutritional assessment)
Psychological evaluation to assess mental readiness
Dietary changes: Patients may be required to follow a liquid diet 1-2 weeks before surgery
Fasting: No food or drink 12 hours before surgery
Lifestyle Adjustments
Stop smoking at least 6 weeks before to promote healing
Reduce alcohol and caffeine intake
Start a healthy eating and exercise routine to ease the transition
Step-by-Step Description of the Procedure
How the Procedure is Performed
Laparoscopic surgery (small incisions in the abdomen)
About 75-80% of the stomach is removed, leaving a narrow tube-like structure
The remaining stomach is stapled closed
Type of Anesthesia Used
- General anesthesia (patient is fully asleep)
Typical Duration of the Procedure
1-2 hours
1-2 day hospital stay after surgery
Risks and Potential Complications
Common Side Effects & Recovery Symptoms
Nausea, vomiting, and acid reflux
Fatigue and weakness in the first few weeks
Temporary hair thinning due to rapid weight loss
Possible Complications & Management
Bleeding or infection (managed with antibiotics or minor procedures)
Staple line leakage (rare but serious; requires immediate medical attention)
Nutritional deficiencies (managed with lifelong vitamin supplements)
Risk Factors
Advanced age, heart conditions, uncontrolled diabetes, and poor pre-operative health can increase risks
Recovery and Aftercare
Recovery Timeline
Hospital stay: 1-2 days
Return to light activities: Within 1-2 weeks
Full recovery: Around 4-6 weeks
Post-Procedure Pain Management
Mild to moderate pain, managed with prescribed medications
Activity Restrictions
No heavy lifting or strenuous exercise for 4-6 weeks
Gradual return to exercise under doctor’s guidance
Follow-Up Appointments & Monitoring
Regular check-ups at 1, 3, 6, and 12 months, then annually
Lifelong commitment to nutritional monitoring
Long-Term Outcomes and Lifestyle Considerations
Permanent or Temporary Results?
- Permanent with the right lifestyle changes
Lifestyle Changes Required
Smaller portion sizes due to reduced stomach size
Nutrient-dense diet to prevent deficiencies
Regular exercise to maintain weight loss
Maintenance & Ongoing Care
Daily vitamin and mineral supplements (B12, iron, calcium, and vitamin D)
Regular medical check-ups to monitor progress
Frequently Asked Questions (FAQs)
Additional Patient Resources
Additional Patient Resources
American Society for Metabolic and Bariatric Surgery (ASMBS): asmbs.org
National Institutes of Health (NIH): nih.gov
Mayo Clinic – Gastric Bypass: mayoclinic.org
Support forums and local bariatric programs can offer peer guidance and ongoing motivation.
